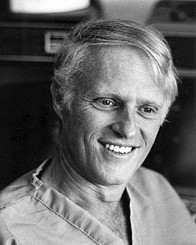
Home » In memoriam » Fred J. Epstein
Fred J. Epstein
1937 – 2006
Message from Dr. Rick Abbott
t is a great honor to speak to you about Fred’s career in pediatric neurosurgery for he will forever be remembered as one of our giants. In academic medicine we are called upon to be an administrator, research clinician and teacher. It is unusual for a person to excel at all three and when they do we speak of the triple threat. Fred was a triple threat.
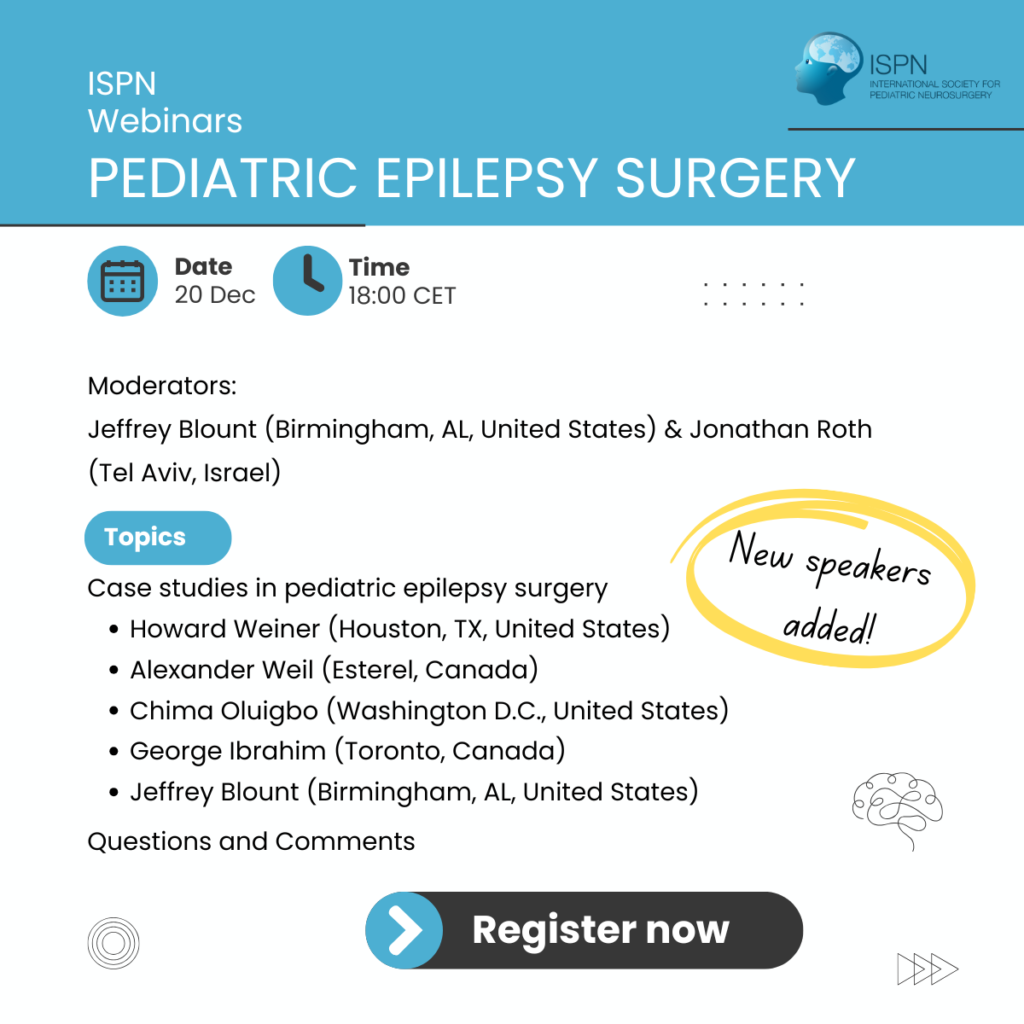
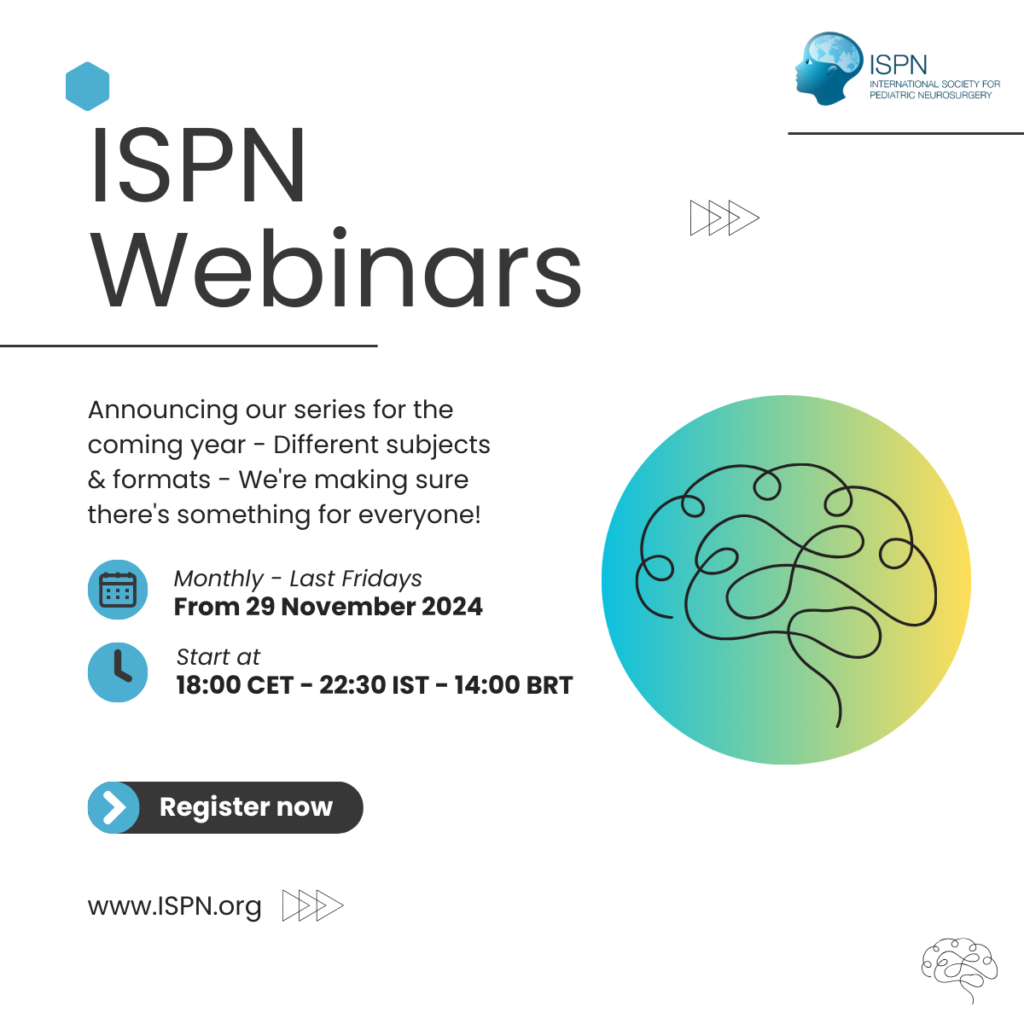
Fred joined the department of neurosurgery at New York University in 1970 and was given the responsibility for treating children. He nurtured his practice and it grew to international preeminence. In 1985 he established the Division of Pediatric Neurosurgery at New York University. Eleven years later he was instrumental in establishing a center of excellence for the neurosciences, a center that again grew to international preeminence largely because of him. Along the way he recruited many physicians to work along side him. It speaks to his ability as a leader that many of these physicians became leaders in their fields, working as Fred did to deliver the highest level of care to children. Fred was a father and not a competitor. Fred also always knew where the buttons were that needed to get pushed so our service had what it needed to care for our young patients. Fred spent a great deal of time working for the acceptance of pediatric neurosurgery as a subspecialty of neurosurgery. He served as the chairman of the Pediatric Section of the American Association of Neurological Surgeons and Congress of Neurological Surgeons, president of the American Society of Neurological Surgeons and president of the International Society for Pediatric Neurosurgery. He was instrumental in the establishment of the American Board of Pediatric Neurological Surgery and served as one of its first Directors accrediting physicians trained in pediatric neurosurgery. His work has lead Pediatric Neurosurgery to becoming a model for other subspecialties of Neurosurgery for training and accrediting their physician specialists.
Fred was also an innovator. Early in his career he participated in the development of a revolutionary piece of equipment that would later be so important for removing tumors in the brainstem and spinal cord. This instrument, the Cavitron, emitted ultrasonic waves that would liquefy tumor without disturbing surrounding tissue. It allowed a surgeon to remove tumors in delicate areas of the nervous system that had previously been considered out-of-bounds. In the late 1970’s a young boy with a tumor in his spinal cord came to him. Fred removed the tumor and the boy recovered his strength. It was with this case that Fred embarked on his mission to explore the boundaries of surgery within the nervous system. By the time I joined him to complete my training he had operated on approximately 40 tumors of the spinal cord and a handful of tumors within the brainstem. I marveled at his mastery. I remember asking him at the completion of the removal of a young child’s spinal cord tumor just how he knew when the removal was complete and how he knew when to stop short to avoid injuring his patient. His reply was “you just know”. My response was I would never do such a surgery, rather I would send my patients to him – I simply could not learn what Fred knew. Fred’s true greatness came in his realizing this and then supporting the development of intraoperative monitoring of the nervous system’s health during tumor removal. During the 1990’s the frontiers of monitoring were pushed back in Fred’s operating room. By the late 90’s criteria had been establish that were predictive of permanent injury with 100% reliability. I remember one Christmas holiday when a child arrived with a tumor in her brainstem. Fred was vacationing in Florida. I called him and he told me to prepare the child for surgery the next day. He would fly up to do the surgery. I watched the next day as he skillfully removed the tumor. At one point the monitoring changed for the worse coming close to predicting injury. Fred stopped his removal of tumor. The monitoring recovered and he proceeded to complete the tumor’s removal. When the surgery was over I asked him why he had come up from Florida given the reality that monitoring had guided the surgery for this child. He acknowledged the importance of the monitoring and that he had not really needed to come, that any of us could have performed the surgery. Fred had moved the surgery for brainstem and spinal cord tumors from an art form that only he had mastered to a surgery that most could accomplish when using the monitoring he helped develop. Fred had assured that surgery would always be available to children with brainstem and spinal cord tumors.
Fred’s greatest gift to us was his teaching. His approach was that of a gentle father with great wisdom. He never taught through intimidation, never belittled and was never condescending. He was quick to share excitement over a new discovery and would without hesitancy support any project that would advance our care of children. I remember going to him early in my fellowship training to speak with him about a surgery being done in France to treat spasticity. I thought it might be interesting to write the surgeon and hoped that Fred might know him. Fred’s response was to tell me to go see him and to take my wife. The result was the introduction of this surgery in New York and its subsequent evolution into a surgery for spasticity of the arm, something not previously available. Fred’s love for pediatric neurosurgery was infectious. During my time at New York University with him it seemed as if nearly every resident left our service with plans on becoming a pediatric neurosurgeon and 8 in the end did. In 1986 Fred established a fellowship for post-residency training in Pediatric Neurosurgery. 21 neurosurgeons have completed this fellowship with Fred and they are now practicing in North America, Europe, the Middle East and Asia. 10 are presently or have been directors of Divisions of Pediatric Neurosurgery, 3 have been or are chairmen of Departments of Neurosurgery and one is the Vice Dean of a prominent medical school in North America. Two have established fellowship training programs of their own. I speak for all in saying that Fred remained our teacher until the very end. We would all consult with him and one of us was even in the process of obtaining an appointment for him as a full professor at a major medical school’s Department of Neurosurgery were he had planned to teach and consult. It was a very strange day for me when I was asked to write a letter of recommendation for this appointment, like he needed one.
We will all miss Fred, as will pediatric neurosurgery. He loved our profession and the children we care for. His aggressive pursuit for cure has been passed on to his trainees. Fred, you have challenged us with your incredible legacy but you have also given us the tools to meet this challenge. I promise you and the families that you cared for that we will not let you down. We will take your tools and continue to push the boundaries as you did. Thank you for your gifts and your loving friendship.
Rick Abbott
Message from Dr. George Jallo
My tribute to Fred Epstein. This is one of the most difficult manuscripts or papers that I have had to write in my career. It is much easier for me to write a paper on brainstem or spinal cord tumors, an area he developed and pioneered. Fred was more than just a mentor or another attending neurosurgeon who trained me but a father figure to me.
My first fond recollection of FRED was when I was a junior resident on the pediatric neurosurgery service at NYU Medical Center. I really did not have an interest in pediatric neurosurgery, I pursued a neurosurgery residency to become a Cerebrovascular Neurosurgeon or Skull Base Surgeon. I was just rotating with him for my 6 month pediatric neurosurgery requirement as a part of my residency training. As other residents and fellows who were able to spend several months with him, you realize that he is “infectious”. He had such a presence to all patients, families and medical staff alike. When we made rounds together all families wanted to meet him and speak with him about their son or daughter’s care. This included families with non neurosurgical issues, such as hernias or asthma. He was the true surgeon willing to speak with his patients and other’s patients without hesitation or indignation. He always introduced himself as FRED, not Dr. Epstein, not the chief of pediatric neurosurgery, not a pioneering surgeon who operated on the edge. He had just a simple approach to children, patient care and pediatric neurosurgery. It was quite simple, he instructed his families to call him Fred anytime or anywhere. He did not need to carry a pager, he gave his cell phone or home number to his patients and made himself readily available. He had this easy approach to children, be available and speak in understandable language. He did not speak down to families or the staff, he always sat with them on a chair or the end of the bed and discussed the patient (which was a child) and not just another case or radiographic disease.
On rounds we always had discussions about my training, my future career and goals. It took me 3 months on his service to change my future life. I wanted to become just like FRED, a pediatric neurosurgeon, with exceptional surgical skills, develop innovative approaches to neurological disorders (whether it be hydrocephalus, brain tumors, brainstem or spinal cord tumors) and be the consummate physician. I knew then I would complete my neurosurgery residency, then do a pediatric fellowship with him. I did not want to be just another pediatric neurosurgeon, I wanted to be a Fred Epstein trained pediatric neurosurgeon. He would teach me the surgical nuances for all neurological disease processes, both in and outside the surgicalsuite. He was the master surgeon in the operating room, comfortable in a child’s brainstem, spinal cord or routine supratentorial brain tumor. I believe he taught me how to operate in these previously charted and uncharted territories. However, I am still trying to emulate him in aspects which can not be measured by one’s CV or resume. This is the approach he had for children and his patients.
In addition to training me, he trained many other exceptional pediatric neurosurgeons who are in practice around the world. I do believe that we all echo my opinion that he is THE MAN who shaped our lives and in turn continues to help children all across the world.
Sincerely,
George Jallo, M.D.
Become a member
Join today and become a part of our community